Many questions surrounding the novel coronavirus remain unanswered. But one thing is already clear: the pathogen affects us all, be it in China, Germany, South Africa or the US. Fighting the disease is increasingly carried out at international level. The University of Bonn is part of numerous international networks that operate on very different levels, striving to slow down the wave of infection.
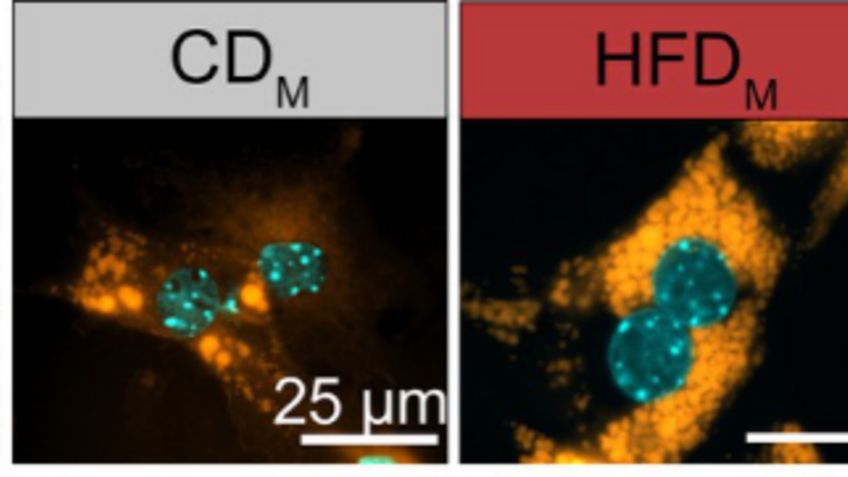
The so-called ACE2 receptor is considered the possible key molecule. It appears that SARS-Coronavirus-2 uses this molecule as a gateway to enter the cell. But which cells produce this receptor in the first place?
And in which way is this production regulated? Members of the HCA Lung Biology Network have been investigating this question over the past weeks. The acronym HCA stands for “Human Cell Atlas,” and the name speaks for itself: cooperating globally, scientists are creating a map of all cell types in the human body, investigating where these cells are formed and how they interact. The Lung Biology Network, of which the University of Bonn is a member, focuses its research on the lungs. The researchers have brought their data together and found that only a relatively small share of the various kinds of pulmonary cells has an ACE2 receptor. Another finding is even more groundbreaking: the production of the receptor is likely supported by interferon.
Interferon is a signal molecule produced by cells upon signs of an infection. Releasing interferon is one of the first defense mechanisms of the human body. Research findings now suggest that interferon causes the exact molecule needed by the virus to enter the cell to reproduce. This could mean that the pathogen benefits from the interferon warning signal, enabling it to infect more cells in less time. Final experiments to confirm these findings are conducted at this instant.
International cooperation is key
The HCA Lung Biology Network is a good example of international cooperation in times of corona. “To contain the pandemic, it is imperative to learn as much as we can about the virus in the shortest time possible”, says Prof. Dr. Joachim Schultze of LIMES (= Life & Medical Sciences) Institute at the University of Bonn, who is also head of the PRECISE Platform for Single Cell Genomics and Epigenomics, a joint venture between the University of Bonn and the German Center for Neurodegenerative Diseases (DZNE). “The only way to achieve this is that researchers cooperate globally.”
The joint research efforts aim at removing the virus from society. The best way to do so is developing an effective vaccine. It will take some time, however, until such a vaccine will be available, and it is likely that many more people will get infected by that time. This is why researchers around the globe are currently also focusing on investigating how to protect patients from the disease progressing severly. “We must better understand the immune system’s reaction to the pathogen and identify patient characteristics and other conditions that may lead to a particularly high risk of falling severely ill,” Schultze stresses. “This is the only chance we have at developing measures that enable us to early identify and prevent the disease progressing in a grave way.” This also relies on the work of experts from many different disciplines, Schultze adds, from clinical experts to virologists, epidemiologists, hygiene specialists, immunologists and geneticists as well as biotechnologists, bioinformaticians, data experts and information scientists.
Which processes cause a severe progression of the disease?
One example of such a cooperation across disciplines is the European LifeTime network. The initiative connects more than 90 research institutions from all over Europe with the common goal of using and further developing state-of-the-art methods from biotechnology and artificial intelligence to answer important questions in the medical field. The LifeTime consortium has created a COVID-19 task force that coordinates the research efforts of involved partners and prioritizes projects depending on urgency and expected findings while ensuring that a certain issue is not worked on by more than one of the involved groups. At the moment, the task force particularly supports researchers in Italy and Spain who are investigating why there are so many cases with a severe progression of the disease in these two countries.
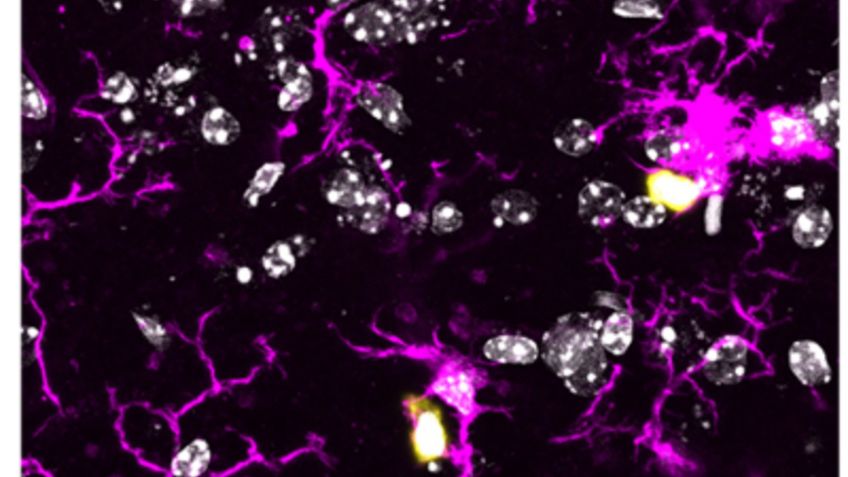
The various impacts COVID-19 can have is indeed striking. But why do some patients seem to be hardly affected by the virus at all while others develop life-threatening forms of pneumonia? There is increasing evidence that the root cause for some of the severe damages caused lies with the immune system itself. What are the reasons behind this? And what other processes contribute to a severe disease progression?
A look inside the genomic library
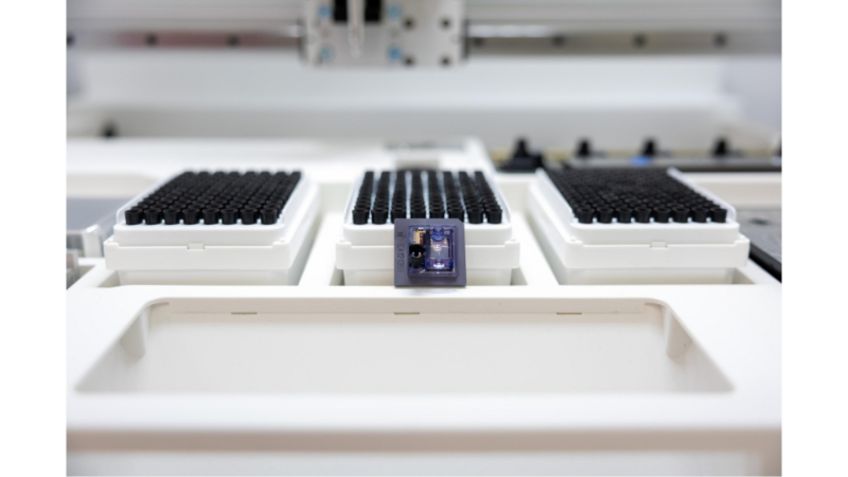
The genes that are deciphered in the course of the disease might give an answer to these questions. There are a number of DFG-founded competence centers in Germany with extensive expertise particularly in this field. The University of Bonn coordinates these so-called NGS (Next Generation Sequencing) centers, which have only recently partnered in a joint COVID-19 initiative. “Among other things, the initiative is trying to find out which genes are especially active in COVID-19 patients over the course of the infection,” Schultze says.
To do so, the experts are extracting so-called RNA from tissue, e.g. from blood samples. Metaphorically speaking, our chromosomes are built like a giant dictionary with tens of thousands of entries. Each entry contains the construction plan of a protein. If a cell needs a protein, it copies the respective entry. This copy is made of RNA. When comparing the RNA molecules formed in different patients, noteworthy observations could be made: for example, certain RNA copies may occur particularly often when the disease progresses severely.
To find out what these particularly active genes actually do, researchers are entering each discovered RNA sequence–put simply: the sequence of letters in the construction plan–into a giant database. This way, they can find out if other studies have already yielded findings on what the gene does. The members of the COVID-19 NGS initiative are planning to make their data accessible to colleagues in other research institutions in Germany, especially to experts that specialize in analyzing large quantities of data. Researchers hope to find that the gene for a particular inflammatory messenger is strongly upregulated in severe cases of the disease–and that there is already a licensed drug that works against that messenger.
Are there different SARS-CoV-2 pathogens?
“Our hope is that this method will enable us to rather quickly identify biological processes that can be stopped with medication,” Schultze explains. Whether this hope can become reality remains uncertain. But even if it doesn’t, the findings will definitely improve our understanding of the infection and our immune response and help complete the coronavirus mosaic.
The sequencing experts of the COVID-19 initiative also work on several other issues: in a total of eight projects, the participating parties want to work on pressing issues related to the disease, e.g. regarding the genome of the virus, the question of whether there are different SARS-CoV-2 pathogens and whether they change genetically, coinfection with other viruses or bacteria, the role of the immune system in modest and severe disease progression, new drugs and, last but not least, the impact of genetic predisposition on the individual risk of infection and disease progression.
Which role do genes play in all this?
Experts in the field of human genetics are also interested in the extent to which we are genetically predisposed for reacting to the pathogen in a certain way. To answer this question, human geneticists of the “COVID-19 host genetics initiative” are examining the entirety of the patients’ genetic information–the genome–to understand the impact of genetic variations in the human body on the probability of developing severe complications. At the University of Bonn, Prof. Dr. Markus Nöthen and his team from the Institute of Human Genetics are working on this matter. They are also very interested in the results of the RNA research described above as it is not unlikely that the conspicuous activity of genes identified in that research is caused by certain mutations. “We want to examine this possibility by sequencing entire patient genomes,” Nöthen explains.
At the moment, the infection rate is receding in many places. Countries like Austria or Denmark have already presented specific plans to ease restrictive measures imposed on public life. Germany is likely to soon start loosening restrictions as well. In the coming months, it will be particularly important to quickly identify and effectively stop a possible second wave of infections. One factor in this process may be monitoring sewage treatment plants. “Along with our Dutch colleagues, we are currently planning to look at the possibility of drawing conclusions from coronavirus residues in sewage as to the infection rate in the population,” explains Prof. Dr. Martin Exner from the Institute of Hygiene and Public Health at the University of Bonn.
Sewage treatment plants as early warning systems for the virus
In this effort, he is closely cooperating with Prof. Dr. Hendrik Streeck from the Institute of Virology and his team, among others. Prof. Streeck and his team are currently conducting extensive analyses on the spread of the infection in Heinsberg–an early hot spot of the coronavirus pandemic in Germany. These analyses have already shown that at least some patients excrete viruses, which do most likely not pose a risk of infection, in their feces. As soon as more detailed results can be presented, we will know the extent to which sewage analyses can yield information as to the exact number of currently infected individuals. “We will most likely have to live with the pathogen for several months or even years,” Exner stresses. “This is why an early warning system like this is very important.” His research partners in the Netherlands have already started testing this kind of sewage analysis.
International networking is also essential in developing disinfection protocols, not least because viruses can become resistant against some agents over time. Furthermore, it remains unclear which routes of transmission are the most crucial: is it really just medium-large respiratory droplets released when coughing or talking? Or do they also include finer aerosols that remain airborne for a longer time before sinking to the ground? And what happens there–on floors, tabletops and other surfaces? For how long do they remain infectious? The answers to these questions will determine the recommended measures for containing the virus. Around the globe, the most important hygiene institutions are regularly updating each other on new findings with regard to COVID-19 and the respective consequences. “This especially includes regulations for check-ups and operations in clinics or medical practices,” says Exner, who is also president of the German Society of Hospital Hygiene (DGKH).
The picture that we have of the pandemic is becoming more complete with each day, and the scientific exchange beyond national borders plays an essential role in this. “In times like these, it is good to see how wonderfully the different teams cooperate even though, under normal circumstances, they may be competitors,” Prof. Dr. Joachim Schultze stresses. The scientific response to the global threat can only benefit from this cooperation, he adds. “These could be regarded as one among the few positive developments resulting from this global crisis.”
Contact:
Prof. Joachim Schultze
LIMES Institute
Genomics and Immunoregulation
Phone 02 28 / 73 - 6 27 87
office.immunogenomics@uni-bonn.de











![[Translate to englisch:] [Translate to englisch:]](/fileadmin/_processed_/e/a/csm_Schultze-IMG_6945-fb_5e6bf9e09f.jpg)