Our lungs are bombarded by all manner of different particles every single day. Whilst some are perfectly safe for us, others—known as pathogens—have the potential to make us ill. The immune system trains its response whenever it encounters such a pathogen. Yet researchers at the University of Bonn have now shown that even harmless particles help to improve the immune response and have published their results in the journal “Nature Immunology.”
An adult takes around 12 breaths a minute, filling their lungs with life-giving air. But they also breathe in all kinds of particles: harmless, germ-free organisms as well as fungal spores and pathogenic bacteria and viruses. “Whether we’re on public transport where people are coughing or in air-conditioned rooms where the air is full of fungal spores, our lungs are constantly being impacted by our environment,” says Professor Andreas Schlitzer, head of the Quantitative Systems Biology working group in the Life & Medical Sciences Institute (LIMES) at the University of Bonn. “It’s a challenge that the immune system in our lungs has to cope with throughout our lives. It has to adapt to ever-changing requirements, distinguish harmless particles from dangerous ones and react accordingly.”
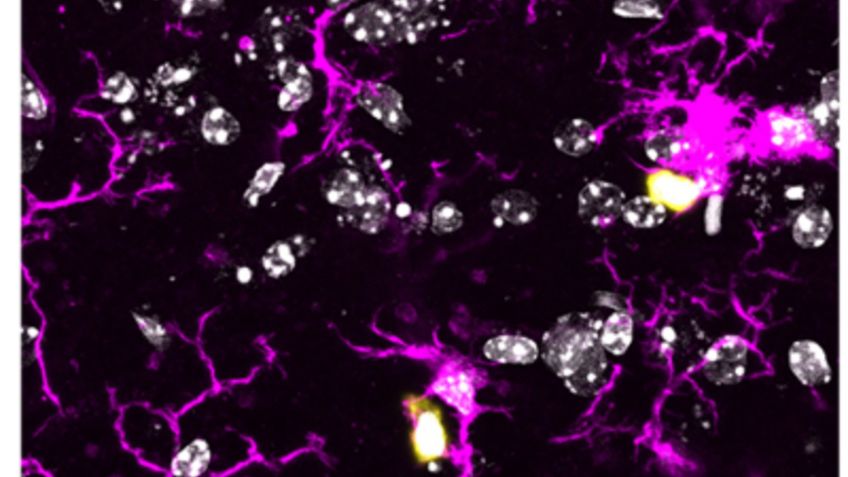
However, the macrophages—cells of the innate immune system that are responsible for this task—know what they have to do. These “scavenger cells” identify pathogenic particles, destroy them reliably—for the most part—and store the attackers’ details in the immune system’s memory so that they can respond even more effectively next time. But what do the macrophages do with information on harmless particles? This was the question investigated by the working group led by Andreas Schlitzer, who is also a member of the Cluster of Excellence ImmunoSensation2 and the Life and Health Transdisciplinary Research Area at the University of Bonn. “The macrophages could simply forget all about innocuous particles because they don’t do us any harm,” Schlitzer explains. “However, we suspected that they retain information on them anyway and incorporate this knowledge into subsequent immune responses.”
Immune response modified by fungal spores
To test their idea, the researchers made mice breathe in beta-glucan, a sugar found inside the cell wall of a fungus called candida. “We’re exposed to these fungal spores all the time in our daily lives,” Schlitzer points out. “You get them in particularly high concentrations inside rooms with air-conditioning, for example, which are ideal places for them to live.” Although this particular fungus is perfectly safe for healthy people, it can put those with a weakened immune system - due to conditions such as HIV, for instance - at risk of serious illness.
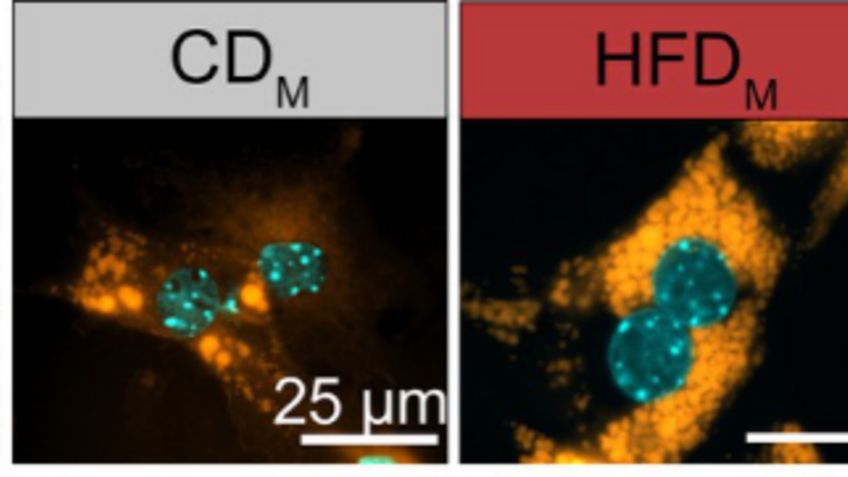
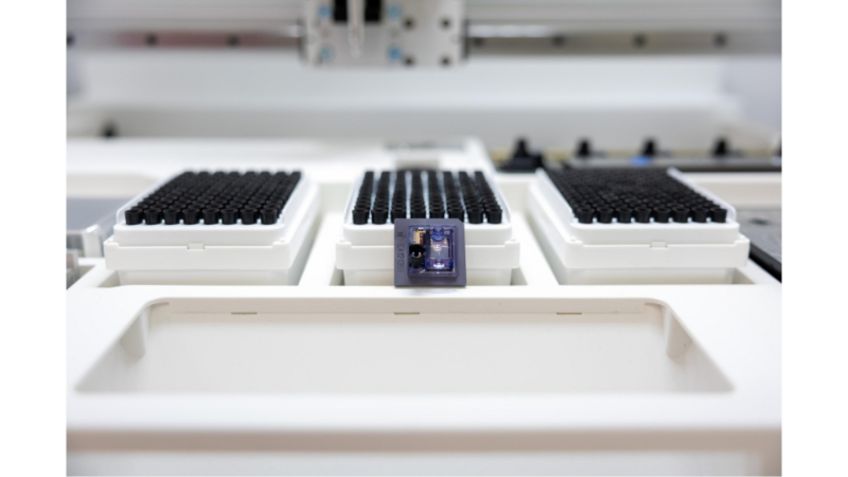
The researchers then used high-dimensional single-cell technologies to study how the mice’s immune system reacted to harmful pathogens. They found that mice that were exposed to the beta-glucan first before being infected with legionella bacteria responded differently to the pathogens than those that were not. “The mice were resistant to the legionella infection or, to put it another way, managed to recover better thanks to their modified immune response,” Schlitzer explains, summing up the findings.
In order to adapt the immune response after coming into contact with harmless particles, macrophages use specific proteins that also play a role in diseases such as Alzheimer’s and obesity. Says Schlitzer: “If we’re able to modulate macrophages in specific ways, they could serve as ‘dials’ that we could tweak in order to treat these conditions.” This is what his working group will be researching going forward.
SPONSORSHIP
Besides LIMES at the University of Bonn, the study also involved the German Center for Neurodegenerative Diseases (DZNE), ETH Zurich, the Technical University of Munich, the University of Edinburgh, Heinrich Heine University Düsseldorf, the University of Zurich, the University Medical Center Hamburg-Eppendorf, the Bernhard Nocht Institute for Tropical Medicine, the Shanghai Institute of Immunology, the University Hospital Schleswig-Holstein, the University of Exeter, East Tennessee State University, the Singapore Immunology Network and the German Center for Infection Research.
It was funded by various sources: an Emmy Noether Research Grant from the German Research Foundation (DFG); Collaborative Research Center 1454 Metaflammation and Cellular Programming; the Diet–Body–Brain (DietBB) research cluster; the European Research Council (ERC); the Wellcome Trust; the Medical Research Council Centre for Medical Mycology at the University of Exeter; a Sir Henry Dale Fellowship jointly awarded by The Wellcome Trust and the Royal Society; the Swiss National Science Foundation, the US National Institutes of Health (NIH); and a UK Research and Innovation (UKRI) Postdoctoral Fellowship Guarantee.
PUBLICATION
Theobald H.1, Bejarano D.A.,1, Katzmarski N.1, Haub J.1, et al., “Apolipoprotein E controls Dectin-1-dependent development of monocyte-derived alveolar macrophages upon pulmonary β-glucan-induced inflammatory adaptation,” in: “Nature Immunology,” 2024. DOI: 10.1038/s41590-024-01830-z
https://www.nature.com/articles/s41590-024-01830-z
CONTACT
Prof. Dr. Andreas Schlitzer
Life & Medical Sciences Institute (LIMES)
University of Bonn
Phone: +49 228 73-62738
Email: aschlitz@uni-bonn.de